As a college junior, I got an ominous call from my mother one day. Dad had gone in for a routine colon screening and wound up with a cancer diagnosis. Mercifully, his malady was confined to a set of polyps that the gastroenterologist removed skillfully. Other than the inconvenience of more frequent screenings, he was expected to live a normal life. Mom informed me that as his progeny, I could expect to have this family history influence my diagnostic screenings.
Fast forward a few decades and a high school friend of mine wound up with colon cancer. Unlike my father, he had not gone in for any screenings until he experienced abdominal pain and bleeding. He was diagnosed with Stage IV colon cancer and died within a year and a half, leaving a wife and two young children. He was a great guy. I can begin to tell you how sad I felt about his predicament.
Colorectal cancer is a silent killer, yielding few (if any) symptoms in the early stage of the disease. It typically starts as small, benign clumps of cells (polyps) that turn malignant over time. As they grow, afflicted individuals may notice changes in their bowel habits, rectal bleeding, abdominal discomfort, weakness, fatigue, and/or weight loss. However, their symptoms may come on so gradually that they fail to pay the appropriate attention to them and take action.
The American Cancer Society estimates that 106,180 new cases of colon cancer and 44,850 new cases of rectal cancer were diagnosed in 2022. Risk factors include age, genetic predisposition, family history, personal history of colorectal cancer or polyps, inflammatory intestinal condition, diet (low fiber, high fat), sedentary lifestyle, diabetes, obesity, smoking, and alcohol abuse. When caught early, 9 out of 10 folks can expect to survive at least 5 years. That’s why screening is so important!
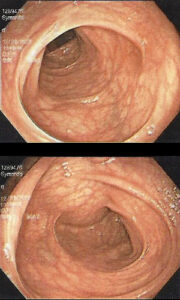 Given my family history, I take colorectal screening seriously. I went in for my colonoscopy just last week. During this procedure, a gastroenterologist uses a long, flexible, tubular instrument to explore the length of the colon. It blows air into the colon to expand its field of vision and transmits images back to the doctor. If he or she detects abnormal tissue, it can be extracted and sent to a laboratory for analysis. An anesthesiologist sedates the patient during the procedure and monitors vital signs throughout. In my experience, the only discomfort occurred with the placement of the IV in my wrist and the injection of the sedative, both of which were transient.
Given my family history, I take colorectal screening seriously. I went in for my colonoscopy just last week. During this procedure, a gastroenterologist uses a long, flexible, tubular instrument to explore the length of the colon. It blows air into the colon to expand its field of vision and transmits images back to the doctor. If he or she detects abnormal tissue, it can be extracted and sent to a laboratory for analysis. An anesthesiologist sedates the patient during the procedure and monitors vital signs throughout. In my experience, the only discomfort occurred with the placement of the IV in my wrist and the injection of the sedative, both of which were transient.
Of course, one must empty one’s intestinal tract of all materials to give the doctor a clear look at the lining of the colon. That’s the “fun” part of the whole ordeal. My latest prep entailed:
- Seven days without nuts, seeds, or whole grains in my diet
- No dietary supplements for seven days (though prescription medications were AOK)
- A clear liquid diet the day before my procedure
- Use of SuTab tablets to induce diarrhea – 12 at 6:00pm the night before and 12 at 4:30 the day of my procedure consumed with a gaggle of water
- Nothing by mouth after 6:30am
My pre-procedure evening wasn’t all that pleasant, and I didn’t get a whole lot of sleep. But the stuff worked exactly as they’d said it would. My check-in time was 9:30am for a 10:30am procedure; I was out of there by 11:30am. My darling husband provided transportation services as the sedative rendered me ill-equipped to operate machinery or make critical decisions.
Suffice it to say, I wouldn’t invest a whole blog post on the subject of colonoscopies if I didn’t believe in their ability to save lives. The CDC recommends that persons 45 and older get screened. If coloscopies aren’t advised, CT colonography, flexible sigmoidoscopy, and/or stool test might prove insightful. A frank discussion with a primary care provider can shed light on one’s individual circumstances. I dearly wish that my high school friend had availed himself of that.
Of course, cancer prevention should also be top of mind. The Mayo Clinic offers the following guidelines for lifestyle choices to reduce the risk of colorectal cancer:
- Eat a high fiber diet with plenty of fruits, vegetables, and whole grains
- Drink alcohol in moderation (if at all).
- Don’t smoke.
- Get at least 30 minutes of exercise daily.
- Maintain a healthy weight.