Healthcare has been a hotbed of activity in our nation’s capital for years. While everyone acknowledges the escalating costs of medical treatment, the debate always seem to center on the economics and allocation of healthcare services. Our elected representatives avoid the more pressing question: Why are Americans so sick?
 Dr. Jeffrey Bland of the Personalized Lifestyle Medicine Institute takes aim at the matter in The Disease Delusion: Conquering the Causes of Chronic Illness for a Healthier, Longer, Happier Life. Chronic illness gives rise to runaway healthcare costs and blunts human vitality. Unfortunately, the prevailing medical protocols treat symptoms with invasive procedures and prescription drugs rather than get to the root cause of the problem. As such, patient conditions progress, and the prescription drugs they take may produce adverse collateral effects.
Dr. Jeffrey Bland of the Personalized Lifestyle Medicine Institute takes aim at the matter in The Disease Delusion: Conquering the Causes of Chronic Illness for a Healthier, Longer, Happier Life. Chronic illness gives rise to runaway healthcare costs and blunts human vitality. Unfortunately, the prevailing medical protocols treat symptoms with invasive procedures and prescription drugs rather than get to the root cause of the problem. As such, patient conditions progress, and the prescription drugs they take may produce adverse collateral effects.
According to Dr. Bland, chronic illness is the result of an imbalance in one or more of the following core physiological processes:
Assimilation and Elimination: Most of us are aware of the fact that what we eat determines nutrient availability for our bodies. We need a healthy gut to extract vital nutrients while creating a barrier against toxic substances that might otherwise leak into our bloodstream. What we may not realize is that the gut also produces and secrets messenger substances that impact a multitude of physiological functions. When any part of this complex system is thrown off kilter by a poor diet or food allergens, chronic disease may result. Solution: Identify/remove food sensitivities, bolster digestive enzymes, and ingest proper nutrients through diet and supplements.
Detoxification: Our livers take responsibility for processing toxins and preparing them for safe elimination. These toxins can be introduced from the outside or take the form of a metabolic byproduct from normal cellular function. Problems arise when the total load of toxins outpaces the liver’s processing capacity. Solution: Minimize environmental toxins and support detoxification with pro-detox foods (e.g., green tea, turmeric, cruciferous vegetables, watercress, cranberry, pomegranate, red grapes.)
Defense: Our immune system takes responsibility for identifying pathogens and eliminating them from our bodies. To perform effectively, it monitors what we eat and what we experience in the environment and stands ready to go on the offensive. A genetic predisposition combined with one or more “triggers” and a leaky gut may cause an autoimmune response – i.e., an attack on the body’s own tissues. Solution: Identify/eliminate triggers and repair leaky gut through diet and lifestyle changes.
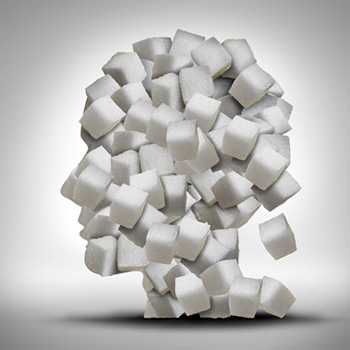
Cellular Communication: Cellular messaging manages interdependencies among core physiological processes. Chronic inflammation alters cellular communication, causing imbalances in the hormones that circulate in the bloodstream. It can manifest as chronic sleep problems, mood swings, fatigue, inability to concentrate, and anxiety. Solution: Identify and eliminate sources of inflammation in the environment, diet, and lifestyle. Consume foods rich in flavonoids and polyphenols to prevent inflammation (e.g., nuts, berries, garlic, onion, grapes, citrus, green tea).
Cellular Transport: The nutrients we ingest must find a way to nurture all of the cells in the body. Protein (as amino acids and albumin) and carbohydrate (as glucose) can be carried by the bloodstream directly. Low Density Lipoproteins (LDLs) transport fat and fat-soluble vitamins (A, D, E, and K) to the cell wall; High Density Lipoprotein (HDL) retrieves the LDL and returns it to the liver. All of these elements need to be in balance for the body to function properly. Solution: Eat a balanced diet based primarily on whole (not processed) foods. Engage in regular aerobic exercise to raise HDL and lower LDL.
Energy: The mitochondria in our cells transform the end products of digestion into energy. Too many calories over too long a period cause mitochondrial burnout. Excess stress for prolonged periods and aging also diminish our production capacity. Solution: Limit caloric consumption using a predominantly plant-based diet. Engage in aerobic and anaerobic exercise regularly to stimulate mitochondrial production.
Structure: We need proper alignment of our bones, muscles, and nerves to function at peak efficiency. Imperfect alignment gives rise to excess wear-and-tear and pain. We also need a proper amount of body fat. Abdominal fat increases the risk of type 2 diabetes, heart disease, stroke, dementia, kidney disease, and breast and prostate cancer. Solution: Bone health requires good nutrition, weight bearing exercise, good digestion, no (or minimal) inflammation, and proper insulin functioning. FYI – Dr. Bland is a fan of the Mediterranean Diet.
 When treated by a functional medicine practitioner, doctor and patient form a partnership to ferret out the root cause of disease and develop a personalized solution based on changes in environment, diet, and lifestyle. This process may entail some trial-and-error to determine what suits the individual’s unique physiology. The physician must be attuned to the patient’s feedback; the patient knows best about his or her condition and the impact of certain therapies and interventions. The partnership works when the parties share knowledge and divide authority. While the treating physician can provide expert guidance, the patient must take responsibility for making the requisite changes to improve health outcomes.
When treated by a functional medicine practitioner, doctor and patient form a partnership to ferret out the root cause of disease and develop a personalized solution based on changes in environment, diet, and lifestyle. This process may entail some trial-and-error to determine what suits the individual’s unique physiology. The physician must be attuned to the patient’s feedback; the patient knows best about his or her condition and the impact of certain therapies and interventions. The partnership works when the parties share knowledge and divide authority. While the treating physician can provide expert guidance, the patient must take responsibility for making the requisite changes to improve health outcomes.