In 1955, American physiologist Ancel Keys delivered a presentation to the World Health Organization that linked coronary artery disease (CAD) to blood serum cholesterol based on epidemiological data from seven industrialized nations. His research turned the tide of American eating habits away from saturated fats toward diets rich in protein and carbohydrates.
British physiologist and nutritionist John Yudkin was not convinced that eliminating saturated fats from the diet would lower rates of CAD. For one thing, two independent examinations of epidemiological data from 20+ industrialized countries failed to support Dr. Keys’ findings. Since affluent populations tend to consume more fat and sugar, smoke more, and lead more sedentary lives, one could argue perhaps that all of these factors contribute to CAD, not just fat consumption. Moreover, Dr. Yudkin claimed that no one has been able to demonstrate that people with CAD on average consume more fat that people without it. He did, however, have his suspicions about the relationship between sugar and CAD, and chased that theory by conducting his own research and reviewing a host of studies by peers.
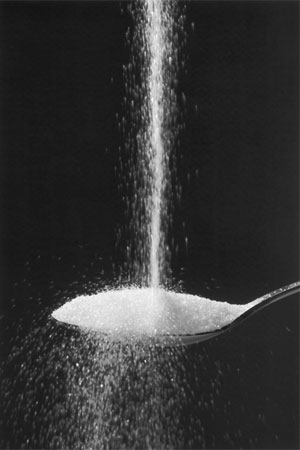
 Yudkin published his findings in Pure, White, and Deadly: How Sugar is Killing Us and What We Can Do to Stop It, my latest bedside read. The book warns that excess consumption of sugar produces a host of unpleasant biological responses that are detrimental to our health, including:
Yudkin published his findings in Pure, White, and Deadly: How Sugar is Killing Us and What We Can Do to Stop It, my latest bedside read. The book warns that excess consumption of sugar produces a host of unpleasant biological responses that are detrimental to our health, including:
- Elevated blood serum cholesterol and triglycerides
(How about that? Sugar holds the smoking gun on cholesterol!) - Hormonal imbalance cause by increased blood serum levels of insulin, cortisol, and estrogen
- Increased “stickiness” of platelets
- Increased acidity and digestive activity of the gastric juices
- Enlargement of the liver and kidneys
- Elevated risk of CAD, hypertension, diabetes, insulin resistance, gall stones
- Tooth decay
Dr. Yudkin also theorized that excess sugar interferes with the balance of good and bad bacteria in the gut microbiome – a theory that has subsequently proven correct.
Dr. Yudkin is quick to point out that his research on sugar should not give rise to a new wave of simplistic advice regarding CAD. People with coronary artery disease tend to have multiple “disturbances” that impact their conditions – e.g., genetic predisposition, unhealthy diets, excess body fat, tobacco use, physical inactivity, stress. So giving up sugar is not a “silver bullet”… even though abstinence comes highly recommended.
So with all this bad news regarding sugar, why do we eat so much of it? One clear answer lies in the fact that sugar tastes good. It makes foods highly palatable and motivates us to eat more and more of it. As such, U.S. food manufacturers have found ways to add sugar into nearly everything they produce. Is it any wonder that our per capita sugar consumption is skyrocketing?
A second major factor lies in the fact that most of us are unaware of how much sugar we’re eating. Very little of Americans’ daily sugar intake comes from table sugar. Most of us aren’t diligent about reading labels and may not even recognize the various forms of sugar that are listed there. And, we may be so used to food tasting sweet that we don’t even register the presence of sugar anymore.
The good news: If you choose to eat whole foods, you won’t have to worry about reading labels, and you won’t ingest hidden quantities of sugar, salt, or fat. And as I’ve learned over the past couple of years, there are lots of ways to make whole foods highly palatable while benefitting from all that good nutrition. Once you’ve broken the sugar cycle, you’ll start to notice all the subtle flavors… and, perhaps, not miss it so much.